TMS and ECT are brain stimulation therapies used to treat certain mental disorders. Both techniques suit patients who show little to no improvement with traditional medication.
If you are considering brain stimulation therapies, it would be best to understand how each one works and if it suits you. You may also be concerned about the advantages of one over the other. Or you may worry about any possible risks and side effects.
In this article, you’ll be able to distinguish between TMS vs. ECT, understand what each therapy involves, and get an informative comparison of both treatments.
ECT vs. TMS
Should you choose ECT? Or is TMS a better option? Before you decide, learn why brain stimulation therapies can be your lifeline.
Medical practitioners may prescribe brain stimulation when patients fail to respond to medication and psychotherapy. Before they do, they must perform a medical exam and schedule sufficient consultation sessions to learn about the patient’s treatment history.
Among the several ways available for brain stimulation are TMS and ECT. Let’s find out how these work.
What Does ECT Mean?
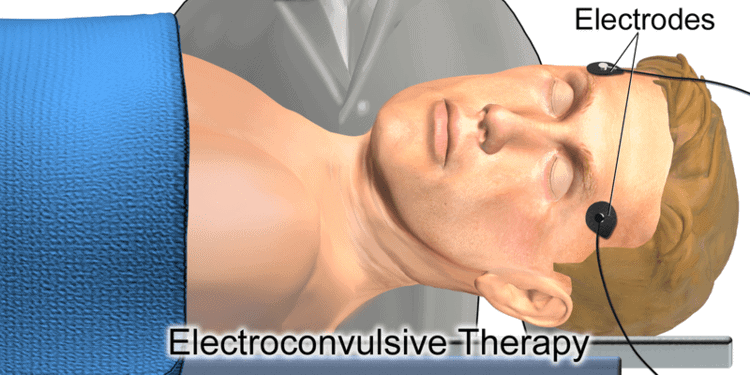
ECT is short for Electroconvulsive Therapy. A psychiatrist delivers electric shocks to the brain briefly to stimulate it.
During the procedure, electrodes are placed on the scalp. These electrodes release controlled electric current into the brain.
Shocks delivered to the brain cause temporary seizures, helping patients find relief from otherwise dangerous symptoms. For instance, if a professional strongly feels that the patient is in danger of committing suicide or hurting themselves, they may turn to ECT to save their life.
Mental health practitioners can use ECT to treat major depressive disorder, bipolar disorder, and other mental conditions.
Because of the violent nature of ECT, it’s a more complicated procedure than TMS. The use of anaesthesia requires that the patient has some downtime after each session before being fully conscious.
What is ECT Therapy?
Electroconvulsive therapy is not a single-session treatment. It takes days, sometimes weeks, to complete, depending on the patient. The therapy typically lasts six to twelve sessions. However, the doctor may vary the length and intervals between treatments according to how individual patients respond to the procedure.
An anesthesiologist will administer general anaesthesia at every session so the patient doesn’t have to deal with seizures. Muscle relaxants also help keep them from moving during the procedure.
Expect to wake up after five to ten minutes after the treatment. Afterward, you can usually go home and continue your daily routine.
You should fully understand and agree to any medical procedure your health practitioner recommends. That’s especially crucial when undergoing brain stimulation of any kind.
Having been in use for decades, scientists agree that ECT’s most common side effects are:
- Short-term memory loss.
- Difficulty learning.
- Risks associated with anaesthesia such as nausea, fatigue, confusion, etc.
- Lasting memory gaps.
It’s necessary to note that most of these side effects appear and disappear after each session.
What Does TMS Mean?

Transcranial Magnetic Stimulation (TMS) is a milder form of brain stimulation than ECT. It uses magnetic fields to activate the brain nerves that regulate patients’ moods.
TMS is repetitive, hence the name rTMS (or repetitive TMS).
Patients sit comfortably in a chair during the procedure. There’s no need for anaesthesia because TMS is painless and doesn’t cause seizures.
During a TMS session, the medical practitioner will place an electromagnetic coil in a predetermined position near the forehead. They then release brief pulses across the skull into the brain.
Treatment typically lasts six weeks with a total of 36 sessions. However, the procedure is highly personalized to suit every patient’s needs. Your physician will determine how much stimulation to use when treating you.
The sessions take only 20 minutes, so they rarely interfere with a patient’s daily activities.
Because of the non-invasive nature of TMS, documented severe risks are rare. However, patients may expect:
- Headaches
- A tingly sensation on the face,
- Lightheadedness
Such reactions usually go away within a short time.
Does TMS Work?
TMS works. Aside from the apparent pros, such as no use of anaesthesia, quick sessions, no downtime, etc., TMS has helped severe depression patients get well.
Thus far, the FDA has approved the treatment of TMS for OCD and TMS for depression. You can trust that it’s safe and efficient. Still, you need to speak with your doctor to determine if TMS suits you.
Transcranial Magnetic Stimulation vs. ECT
While TMS and ECT are welcome options for patients with non-responsive mental conditions, each has pros and cons.
We’ve noticed that many patients prefer TMS over ECT. Often, such patients cite the advantages of TMS, such as:
- Staying conscious during the procedure
- No seizures
- Limited stimulation
- No recovery time is necessary
- It’s non-invasive
- TMS is painless
- Milder side effects, etc.
We concur. Knowing how challenging life can be when depression doesn’t respond to medication, we offer TMS to help our patients.
If you think TMS can help you, visit us at our transcranial magnetic stimulation office or call (617) 431-6140.